Cancer combatants: navigating the frontier of cancer immunotherapy
- Sayasvi Sarathchandran
- Sep 23, 2024
- 4 min read
Immunotherapy[2] is a type of treatment that utilises the body's own immune system to fight diseases such as cancer, autoimmune disorders, and infectious diseases. Unlike traditional treatments like chemotherapy, which directly target the disease, immunotherapy works indirectly by activating or suppressing an immune response that targets abnormal cells. The development of immunomemory as a result can bring about lasting remission. Since this treatment is limited to the immune system only, it has fewer side effects, but also gives a higher risk of developing autoimmune disorders. Currently, immunotherapy can be used to treat cancers of the mouth, throat, larynx, sinuses, nose and salivary glands, either alone or in combination with chemotherapy, radiotherapy and/or surgery, making other such methods more effective. Current immunotherapy types include monoclonal antibodies (including checkpoint inhibitors), CAR T-cell therapy and vaccines; although there has recently been significant research into the tumour microenvironment to make immunotherapy more effective.[4]
Monoclonal antibodies[1]
Monoclonal antibodies (MABs) recognise and target specific proteins on cancer cells. There are many different types of MABs.
Cancer cells produce many growth factor receptors, which send signals that cause the cell to divide. Some MABs block this signal or the receptor itself, to prevent the spread of the tumour.
Conjugated MABs carry drugs or radioactive substances to cancer cells, causing them to undergo apoptosis.
Cancer cells can produce vascular endothelial growth factor (VEGF) proteins that attach to receptors on cells lining the walls of blood vessels within the tumour, which causes the blood vessel, and therefore the tumour, to grow. MABs known as anti-angiogenic drugs block VEGF proteins from attaching to these receptors.
Some MABs attach to cancer cells, so that effector lymphocytes can detect them more easily. This process is known as antibody-dependent cell-mediated cytotoxicity (ADCC). Examples of MABS that work in this way include Herceptin, which is used to treat breast cancer and stomach cancer.
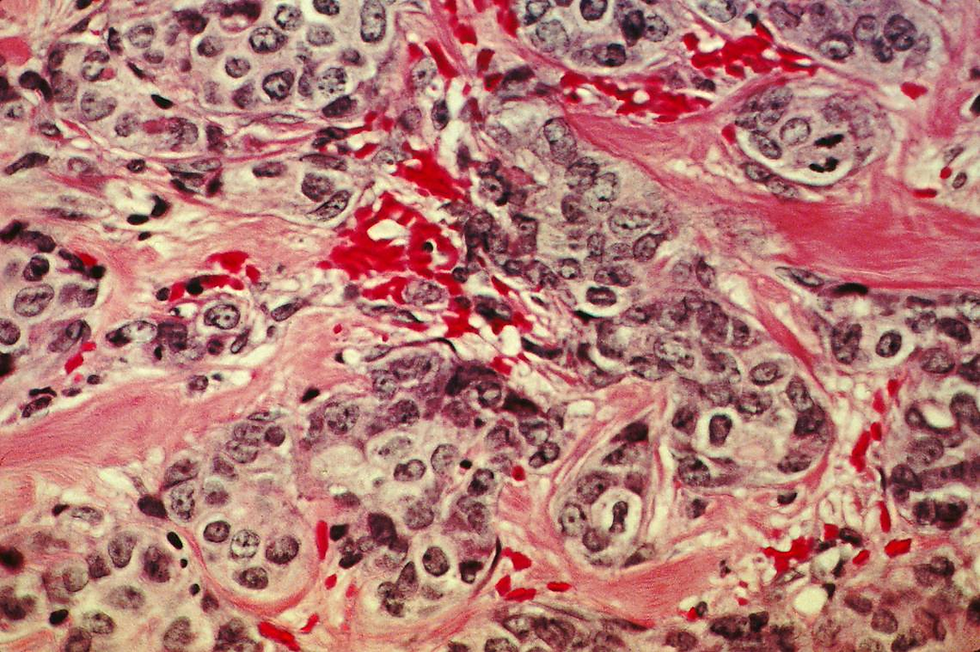
Immune checkpoint inhibitors (ICIs) are MABs that act on the cells of the immune system. ICIs block proteins that stop T cells from attacking cancer cells, thereby interfering with the mechanism that the tumour uses to evade the host’s immune response. Checkpoint inhibitors block different proteins, such as PD-1 (programmed cell death protein 1) and PD-L1 (programmed death ligand 1), as seen in the above image.
Vaccines[2]
Cancer vaccines aim to help the immune system recognise and destroy cancer cells with tumour-associated antigens. They can be formed from proteins or sections of DNA/ RNA strands from cancer cells, or even entire cancer cells, dendritic cells grown alongside cancer cells or viruses. Cancer vaccines can be categorised as either prophylactic (preventative) or therapeutic. Prophylactic vaccines are designed to prevent cancer developing in healthy individuals who are at high risk, by targeting viruses that are known to cause cancers such as HPV and the hepatitis B vaccine. Conversely, therapeutic vaccines activate the immune system of an infected individual, such as the T-VEC vaccine that combats advanced oncolytic melanoma.
CAR T-cell therapy[6]
CAR T-cell therapy can be used to treat children with leukaemia and some adults with lymphoma (but only around 200 adults annually). A sample of T cells from the patient’s blood is genetically engineered into CAR (chimeric antigen receptor) T-cells, to bind to and attack specific cancer cells. They are then cloned and infused into the patient’s bloodstream. This technique has proven to be particularly effective against B-cell acute lymphoblastic leukaemia, with a 80-90% complete remission rate.
Tumour Microenvironment[5][7]
However, with only 20-40% of patients responding to immunotherapy, it is evident that the success of the aforementioned methods is limited to a small minority. This may be attributed to the fact that the causes of resistance to immunotherapy derive not only from the tumour itself, but also from the complex interactions between the tumour and its microenvironment (TME). The TME is composed not only of cancer cells, but also host immune cells, stromal and epithelial tissue and the extracellular matrix. The whole TME experiences environmental changes, such as hypoxia (low oxygen) which can lead to immunotherapy resistance and increased metastasis. The lack of consideration of the TME can inhibit immunotherapy techniques, such as CAR T-cell therapy and cancer vaccines. Modifying the TME, not just the tumour cells in isolation in the design of novel immunotherapy drugs, could be pivotal to increasing the success rate of immunotherapy.
Therefore, it is evident that immunotherapy offers a promising avenue in the treatment of cancer, with techniques ranging from checkpoint inhibitors to genetically modifying T-cells. However, the varying efficacy between patients with such current methods implies the need for further research into other factors that affect immunogenicity, namely the TME. Immunotherapies designed to specifically target the microenvironment could transform our approach to cancer treatments in the future.
Citations
1) Cancer Research UK (2021). Monoclonal Antibodies | Targeted Cancer Drugs | Cancer Research UK. [online] www.cancerresearchuk.org. Available at: https://www.cancerresearchuk.org/about-cancer/treatment/targeted-cancer-drugs/types/monoclonal-antibodies.
2) Cancer research UK (2021). What is immunotherapy| Cancer Research UK. [online] www.cancerresearchuk.org. Available at: https://www.cancerresearchuk.org/about-cancer/treatment/immunotherapy/what-is-immunotherapy.
3) Decoding the signs of response to cancer immunotherapy. (n.d.). www.nature.com. [online] Available at: https://www.nature.com/articles/d42473-019-00064-0 [Accessed 13 Oct. 2021].
4) DEDE, Z., TUMER, K., KAN, T. and YUCEL, B. (2023). Current Advances and Future Prospects in Cancer Immunotherapeutics. Medeniyet medical journal, [online] 38(1), pp.88–94. doi:https://doi.org/10.4274/mmj.galenos.2023.29599.Murciano-Goroff,
5) Y.R., Warner, A.B. and Wolchok, J.D. (2020). The future of cancer immunotherapy: microenvironment-targeting combinations. Cell Research, [online] 30(6), pp.507–519. doi:https://doi.org/10.1038/s41422-020-0337-2.National
6) Cancer Institute (2022). T-cell transfer therapy - immunotherapy. [online] National Cancer Institute. Available at: https://www.cancer.gov/about cancer/treatment/types/immunotherapy/t-cell-transfer-therapy.www.oncology.ox.ac.uk.
7)(n.d.). Tumour Microenvironment. [online] Available at: https://www.oncology.ox.ac.uk/research/tumour-microenvironment [Accessed 25 Mar. 2024].

Comments